A 48 YR OLD FEMALE FARMER BY OCCUPATION RESIDENT OF VELLEMLA CAME WITH CHIEF COMPLAINTS:
WOUND OVER THE LEFT FOOT SINCE 4 MONTHS
HISTORY OF PRESENT ILLNESS:
PATIENT WAS APPARENTLY ASYMPTOMATIC 4 MONTHS BACK, AFTER WHICH SHE DEVELOPED BLACKISH DISCOLORATION OF LEFT GREAT TOE WHICH WAS INSIDIOUS IN ONSET GRADUALLY PROGRESSIVE, ASSOCIATED WITH SWELLING OF THE LEFT LIMB TILL MID FOOT FOR WHICH SHE WENT TO A LOCAL PRACTITIONER AND WAS TREATED WITH DRESSING THERE WAS NO IMPROVEMENT, WITH PROGRESSION OF WOUND, ASSOCIATED WITH FOUL SMELLING DISCHARGE FOR WHICH SHE WAS TAKEN TO AN OUTSIDE HOSPITAL WHERE DIS ARTICULATON OF LEFT GREAT TOE WAS DONE ON 13/04/24
CAME ON LAMA TO OUR HOSPITAL FOR FURTHER MANAGEMENT
NO H/O FEVER,COUGH,COLD.
NO H/O CHEST PAIN, PALPITATIONS, BREATHLESSNESS, ORTHOPNEA, PND.
NO H/O ABDOMINAL PAIN, BURNING MICTURITION, NAUSEA, VOMITING.
DALIY ROUTINE :
WAKES UP AT 6 AM IN THE MORNING
DRINKS TEA AND DOES HOUSEHOLD WORK
HAVE BREAKFAST FAST AT 9 AM
GOES TO THE FIELDS
EATS LUNCH AT 2 PM
DOES WORK IN THE FIELDS(PADDY AND COTTON FIELDS)
DRINKS TEA IN THE EVENING AT 5 PM
DOES HOUSEHOLD WORK
EATS DINNER AT 8 PM
SLEEPS AT 10 PM
DECREASED WORKING ACTIVITIES SINCE 6 YEARS WHEN SHE WAS DIAGNOSED WITH DIABETES
HISTORY OF PAST ILLNESS:
K/C/O TYPE 2 DIABETES MELLITUS SINCE 6 YEARS (ON TAB GLIMI M1/OD)
NO H/O HYPERTENSION, ASTHMA, TB, EPILEPSY, CVA,CAD,CKD,CLD.
TREATMENT HISTORY:
ON TAB.GLIMI-M1 PO/OD
PERSONAL HISTORY:
MARRIED
OCCUPATION: FARMER
APPETITE: NORMAL
DIET: MIXED
BOWEL AND BLADDER: REGULAR
KNOWN ALLERGIES: NO
ADDICTIONS: NO
FAMILY HISTORY:
NO SIGNIFICANT HISTORY,
GENERAL EXAMINATION:
PT IS CONCIOUS, COHERENT AND COOPERATIVE, MODERATELY BUILT AND NOURISHED.
PALLOR PRESENT.
NO ICTERUS, CYANOSIS, CLUBBING, LYMPHADENOPATHY, EDEMA.
TEMP-97.6 F
PR- 86 BPM
RR -18 CPM
BP - 80/50 MMHG
SPO2-98% AT RA
GRBS-164 MG/DL
SYSTEMIC EXAMINATION:
CVS- S1,S2 HEARD, NO MURMURS
RS-VESICULAR BREATH SOUNDS HEARD, NO WHEEZE AND DYSPNEA.NO CREPTS
P/A-SOFT, NON-TENDER, NO ORGANOMEGALY
CNS
LEVEL OF CONSCIOUSNESS : CONSCIOUS
SPEECH: INCOHERENT
SIGNS OF MENINGEAL IRRITATION: NEGATIVE
CRANIAL NERVES: NAD
MOTOR SYSTEM:
UL LL
TONE - NORMAL NORMAL
NORMAL NORMAL
POWER: 5/5 5/5
GLASGOW SCALE: E4 V5 M6
REFLEXES:
Right Left
BICEPS 2+ 2+
TRICEPS 2+ 2+
SUPINATOR + +
KNEE 2+ 2+
ANKLE NOT ELICITABLE +
PLANTARS - FLEXOR
LOCAL EXAMINATION OF LEFT FOOT :
INSPECTION -
ULCER OF SIZE 5×4 CMS OVER THE DORSUM OF THE LEFT FOOT
SURROUNDING SKIN APPEARS TO BE NORMAL
MARGINS ARE IRREGULAR
EDGES ARE SLOPING
FLOOR IS COVERED BY SLOUGH AND GRANULATION TISSUE
PALPATION -
TENDERNESS +
NO LOCAL RISE OF TEMPERATURE
ALL INSPECTORY FINDINGS ARE CONFIRMED
BASE IS UNDERLYING FASCIA AND BONE
COURSE IN THE HOSPITAL:
48 YEAR OLD FEMALE CAME TO CASUALITY WITH CHIEF COMPLAINTS OF WOUND ON LEFT FOOT SINCE 4 MONTH.
PATIENT WAS APPARENTLY ASYMPTOMATIC 4 MONTHS AGO THEN SHE DEVELOPED BLACKISH DISCOLORATION OF LEFT GREAT TOE SINCE 4 MONTHS, INSIDIOUS IN ONSET, GRADUALLY PROGRESSIVE ASSOCIATED WITH SWELLING OF LEFT FOOT
PATIENT INITIALLY WENT TO OUTSIDE HOSPITAL IN HYDERABAD AND GOT DISARTICULATION OF LEFT GREAT TOE ON 13/04/2024 AND WAS ON IONOTROPIC SUPPORT AND WAS MANAGED THERE FOR 4-5 DAYS AND THEY GOT LAMA DISCHARGE FROM HOSPITAL DUE TO PERSONAL REASONS.
AS PATIENT CAME WITH FOLEYS IN SITU, FOLEYS WAS CHANGED ON THE DAY 1 OF ADMISSION AND DE CATHETERISED ON DAY 5 OF ADMISSION.
ON ARRIVAL PATIENT BP-90/50 MMHG WITH NORAD 4 ML/HR
GRBS-165 MG/DL ON INJ. INSULIN HAI SC/TID.
PATIENT WAS ADMITTED IN ICU AND WAS STARTED ON INJ. HAI SC/TID AND INJ. NPH BD ACCORDING TO RBS LEVELS.
IONOTROPES INJ. NORADRENALINE AND INJ. VASOPRESSIN INFUSIONS STARTED AND TITRATED ACCORDINGLY TO MAINTAIN MAP(MEAN ARTERIAL PRESSURE) >65 MMHG.
PATIENT TREATED WITH BROAD SPECTRUM ANTIBIOTICS, NECESSARY INVESTIGATIONS WERE DONE AND BLOOD, URINE CULTURE AND SENSTIVITY SAMPLES SENT AND OTHER NECESSARY INVESTIGATIONS WERE DONE PATIENT WAS STARTED ON DUAL IONOTROPES AND RIGHT IJV TRIPLE LUMEN CATHETERISATION WAS DONE 21/04/24 UNDER ASEPTIC CONDITIONS AND THE PROCEDURE WAS UNEVENTFUL; WOUND DRESSINGS WERE DONE ON REGULAR BASIS AFTER CROSS CONSULTATION WITH GENERAL SURGERY.
GENERAL SURGERY ON 19/04/24 I/V/O DIABETIC ULCER OVER LEFT FOOT:
1. HIGH PROTEIN DIET. (DIABETIC PROTEIN POWDER 2 TBSP IN GLASS OF MILK PO/BD)
2. T.CHYMEROL FORTE PO/TID.
3. BOTH LOWER LIMB ELEVATION.
4. REGULAR ASD(MGSO4 DRESSING FOR LEFT LOWER LIMB).
IONOTROPIC SUPPORT WAS STOPPED ON 23/4/2024 AND PATIENT IS HEMODYNAMICALLY STABLE
BLOOD TRANSFUSION (1 UNIT PRBC) DONE ON 25/04/2024 I/V/O HEMOGLOBIN-7.6G/DL POST TRANSFUSION Hb 10.2 G/DL,
GENERAL SURGERY REFERRAL WAS DONE ON 24/04/24 I/V/O DIABETIC ULCER OVER LEFT FOOT DEBRIDEMENT OF ULCER AND PAPAYA DRESSING DONE.
DURING THE STAY IN THE HOSPITAL, PATIENT WAS ACTIVELY AMBULATED, FROM DAY 4 OF ADMISSION HEALTHY GRANULATION TISSUE WAS FORMED IN THE WOUND PATIENT IS BEING DISCHARGED AS SHE SHOWED SIGNS OF PROGRESSIVE HEALING AND IS HEMODYNAMICALLY STABLE, WITH GLYCEMIC CONTROL.
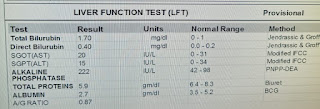
INVESTIGATIONS
19-04-24
20-04-24
21-04-24
22-04-24
23-04-24
24-04-24
25-04-24
26-04-24
27-04-24
28-04-24
29-04-24
URINE FOR CULTURE AND SENSTIVITY:
1-2 PUS CELLS SEEN. PLENTY OF BUDDING YEAST CELLS SEEN.
NON ALBICANS CANDIDA >10° CFU/ML OF URINE.
SWAB FOR CULTURE AND SENSTIVITY:
FEW PUS CELLS, OCCASIONAL GRAM POSITIVE COCCI IN SINGLES SEEN OCCASIONAL GRAM NEGATIVE BACILLI SEEN.
NON ALBICANS CANDIDA ISOLATED.
BLOOD FOR CULTURE AND SENSTIVITY: NO GROWTH AFTER 48 HOURS OF AEROBIC INCUBATION.
USG ABDOMEN DONE ON 20/04/2024:
LIVER-NORMAL S/E NO F/L
PV-NORMAL, NO IHBRD
CBD-NORMAL
GALL BLADDER-DISTENDED WALL THICKNESS-NORMAL
PANCREAS-HEAD VISUALISED, NORMAL S/E
SPLEEN-9.2 CM NORMAL S/E
RIGHT KIDNEY-9.9 X 4.1 CM, NORMAL S/INCREASED ECHOGENICITY, CMD+ LEFT KIDNEY-8.4 X 3.7 CM, NORMAL S/INCREASED ECHOGENICITY,CMD+ AORTA I.V.C. - NORMAL
NO ASCITES
NO LYMPHADENOPATHY U.BLADDER-EMPTY, FOLEYS CATHETER INSERTED. PELVIS COULD NOT BE ASSESSED.
IMPRESSION:
RAISED ECHOGENICITY OF BILATERAL KIDNEYS.
2-D ECHO DONE ON 23/04/2024:
NO RWMA,
TRIVIAL TR+/AR+/MR+
MAC+ SCLEROTIC AV: NO AS/MS.
EF=59%; RVSP=23+10=33MMHG.
GOOD LV SYSTOLIC FUNCTION.
GRADE 1 DIASTOLIC DYSFUNCTION+.
MINIMAL PE+.
IVC SIZE (0.8 CMS) COLLAPSING
PROVISIONAL DIAGNOSIS :
SEPTIC SHOCK WITH MULTI ORGAN DYSFUNCTION (RESOLVED)
SECONDARY TO LEFT DIABETIC FOOT
S/P: DISARTICULATION OF LEFT GREAT TOE (13/04/2024)
K/C/O TYPE 2 DIABETES MELLITUS SINCE 6 YEARS
TREATMENT :
IV FLUIDS NS
INJ.PIPTAZ 4.5 GM/IV/TID
INJ.CLINDAMYCIN 600 MG/IV/BD
INJ.PAN 40 MG/IV/OD AT 8 AM
INJ HUMAN ACTRAPID INSULIN S/C TID PRE-MEAL ACCORDING TO GRBS
INJ NPH S/C BD PRE-MEAL ACCORDING TO GRBS
SYP POTKLOR 15ML PO/BD IN A GLASS OF WATER (I/V/O HYPOKALEMIA)
AMBULATION AND POSITION CHANGE
REGULAR DRESSING OF LEFT FOOT
BP.PR.RR,SPO2 MONITORING 2ND HOURLY